Human IVG Paves the Way for Universal Fertility Treatments

By

Researchers from the Institute for the Advanced Study of Human Biology (WPI-ASHBi) at Kyoto University have made significant strides in human in vitro gametogenesis (IVG). They have successfully identified optimal culture conditions that facilitate epigenetic reprogramming with bone morphogenetic protein (BMP), a key step towards translating IVG technology into clinical settings for infertility treatments. Credit: SciTechDaily
New IVG research offers promising methods for creating human germ cells from stem cells, potentially transforming fertility treatments.
According to the World Health Organization, approximately 1 in 6 people are affected by infertility at some point in their life. The American Society for Reproductive Medicine (ASRM) defines infertility as a condition characterized by the inability to achieve a successful pregnancy, based on factors such as medical, sexual, and reproductive history, age, physical findings, and diagnostic testing, or requiring the use of donor gametes to achieve pregnancy. While assisted reproductive technologies (ARTs) like in vitro fertilization (IVF) have significantly improved treatment for certain types of infertility, not all forms can be addressed with current strategies.
Breakthroughs in Human In Vitro Gametogenesis
A significant advancement in the field is the development of human in vitro gametogenesis (IVG), which uses pluripotent stem cells (PSCs) such as induced pluripotent stem cells (iPSCs) from patients, to generate human germ cells with the capacity to potentially give rise to mature gametes in culture, offering a gateway to treating all form of infertility —independent of gender. Nevertheless, human IVG research remains in its infancy, with the current goal being to reconstitute the complete process of human gametogenesis. To date, one major challenge has been to recapitulate in the founder population of germ cells, or the human primordial germ cells (hPGCs), a hallmark event known as epigenetic reprogramming —in which the inherited parental “memory” of cells, present on its DNA, is reset/erased— that is required for proper germ cell differentiation.
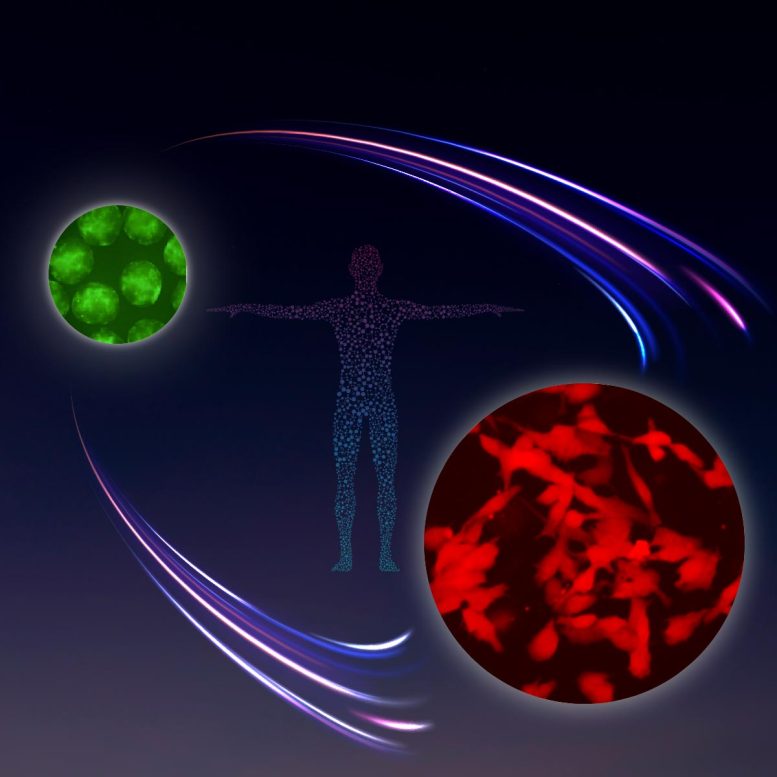
Image inspired by NASA’s Apollo Program, representing the successful in vitro germ cell differentiation from TFAP2C-EGFP +ve human primordial germ cell-like cells (hPGCLCs; labeled in green) to DAZL-tdTomato +ve human mitotic pro-spermatogonia (labeled in red). Credit: WPI-ASHBi/Kyoto University
Recent Developments in Human IVG Research
A team of researchers from the Institute for the Advanced Study of Human Biology (WPI-ASHBi) at Kyoto University have identified robust culture conditions necessary to drive epigenetic reprogramming and germ cell differentiation into precursors of mature gametes, the mitotic pro-spermatogonia and pro-oogonia with the capacity for extensive amplification, achieving a new milestone for human IVG research. The researchers, led by Dr. Mitinori Saitou, have published these revolutionary findings in the journal Nature.
Prior work from Saitou’s team and other groups successfully generated so-called human primordial germ cell-like cells (hPGCLCs) from PSCs in vitro, which recapitulated several fundamental features of hPGC, including the capacity to propagate. However, these hPGCLCs were unable to undergo epigenetic reprogramming and differentiation. These limitations could be bypassed by aggregating hPGCLCs with mouse embryonic (non-germinal) gonadal cells to mimic the microenvironment of the testis/ovary, thereby effectively “reconstituting” the tissue(s). However, this process is inefficient and impractical from a clinical application perspective. Therefore, in order to achieve the ultimate goal of human IVG research, it is essential to identify the minimal culture conditions necessary to generate mature human gametes.

Left: Ryuta Yokogawa, Center: Mitinori Saitou MD. PhD., Right: Yusuke Murase PhD. Credit: WPI-ASHBi/Kyoto University
Significance of BMP in Reprogramming and Differentiation
In their new study, Saitou and colleagues conducted a cell culture-based screen to identify potential signaling molecules required to drive epigenetic reprogramming and differentiation of hPGCLCs into mitotic pro-spermatogonia and oogonia. Surprisingly, the authors found that the well-established developmental signaling molecule, bone morphogenetic protein (BMP), played a crucial role in this reprogramming and differentiation process of hPGCLCs. “Indeed, considering that BMP signaling already has an established role in germ cell specification, it was highly unexpected that it also drives hPGCLC epigenetic reprogramming” comments Saitou.
Remarkably, these hPGCLC-derived mitotic pro-spermatogonia/oogonia not only displayed similarities in gene expression and epigenetic profiles to that of actual hPGC differentiation in our bodies but also underwent extensive amplification (over 10 billion-fold). “Our approach enables near-indefinite amplification of mitotic pro-spermatogonia and oogonia in culture and we now also have the ability to store and re-expand these cells as needed,” says Saitou.
Implications and Future Directions
The authors also revealed the potential mechanisms of how BMP signaling may be leading to epigenetic reprogramming and hPGCLC differentiation. “BMP (signaling) appears to be attenuating the MAPK/ERK (mitogen-activated protein kinase/extracellular-regulated kinase) signaling pathway and both the de novo and maintenance activities of DNMT (DNA methyltransferase), but further investigation will be necessary to determine the precise mechanism and whether this is direct or indirect”, explains Saitou.
“Our study represents not only a fundamental advance in our understanding of human biology and the principles behind epigenetic reprogramming in humans but also a true milestone in human IVG research,” he adds.
Saitou comments, “Although many challenges remain and the path will certainly be long, especially when considering the ethical, legal, and social implications associated with the clinical application of human IVG, nevertheless, we have now made one significant leap forward towards the potential translation of IVG into reproductive medicine.”
Reference: “In vitro reconstitution of epigenetic reprogramming in the human germ line” by Yusuke Murase, Ryuta Yokogawa, Yukihiro Yabuta, Masahiro Nagano, Yoshitaka Katou, Manami Mizuyama, Ayaka Kitamura, Pimpitcha Puangsricharoen, Chika Yamashiro, Bo Hu, Ken Mizuta, Kosuke Ogata, Yasushi Ishihama and Mitinori Saitou, 20 May 2024, Nature.
DOI: 10.1038/s41586-024-07526-6


